Understanding the Risks of Gastrointestinal Leaks in Bariatric Surgery: A Detailed Overview
Bariatric surgery, encompassing procedures like laparoscopic sleeve gastrectomy (LSG) and laparoscopic Roux-en-Y gastric bypass (LRYGB), has become increasingly popular for managing morbid obesity. While these surgeries can lead to significant weight loss and improvement in comorbid conditions, they are not without risks. One of the most concerning complications is a gastrointestinal leak, which, although rare, can lead to severe morbidity and even mortality. This blog post delves into a recent study analyzing the risk factors and interventions related to gastrointestinal leaks in bariatric surgery.
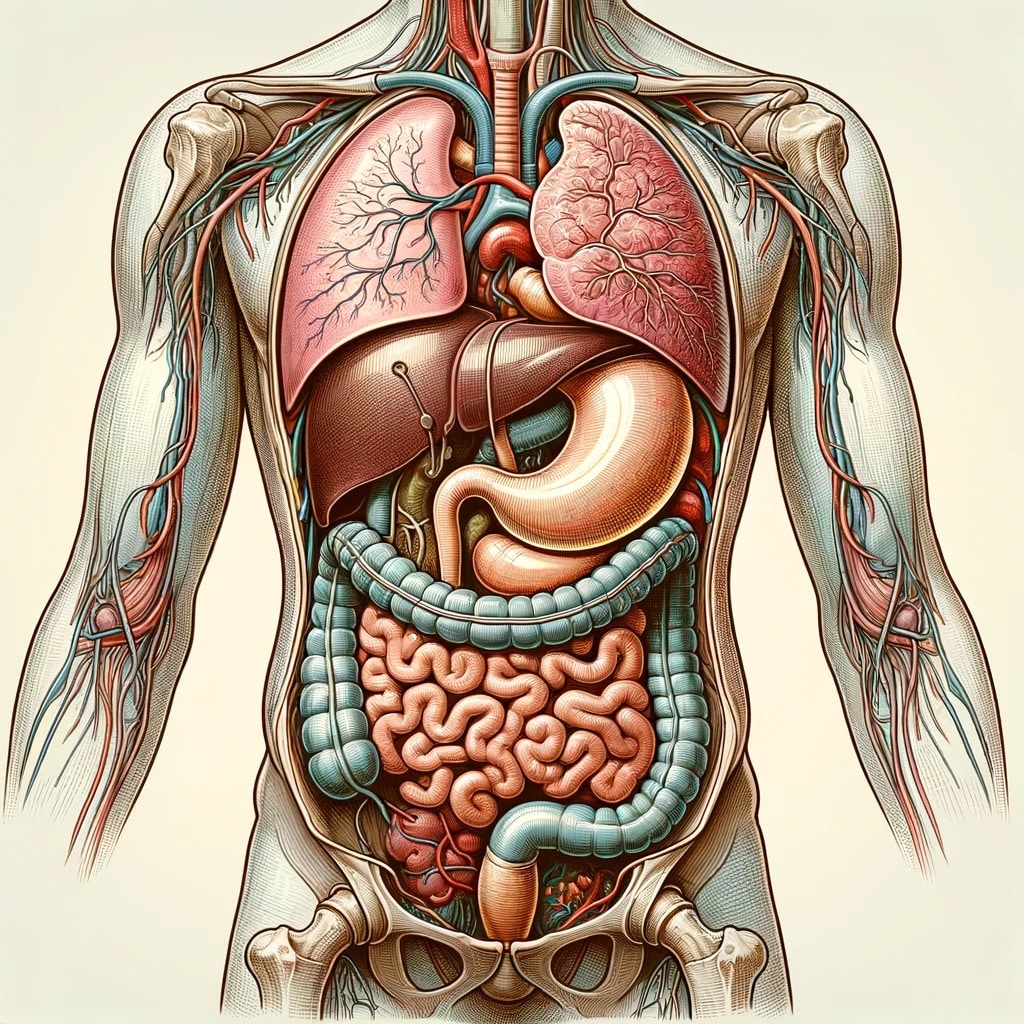
What is a Gastrointestinal Leak?
A gastrointestinal leak occurs when there is an abnormal opening in the stomach or intestinal wall, allowing contents to leak into the abdominal cavity. This can lead to infections and other serious complications. Early detection and management are crucial to mitigate the adverse effects.
Study Overview
A comprehensive study published in the Journal of the American College of Surgeons analyzed data from 133,478 patients who underwent LSG and LRYGB. The study aimed to identify risk factors for leaks and evaluate the impact of common perioperative interventions like intraoperative provocative tests, surgical drain placement, and postoperative swallow studies on the development of leaks.
Key Findings
1. Overall Leak Rate: The study found that the overall leak rate was 0.7%, with a higher incidence in patients undergoing LRYGB compared to LSG.
2. Risk Factors: Several preoperative conditions were associated with an increased risk of leaks, including:
• Oxygen dependency (AOR 1.97)
• Hypoalbuminemia (AOR 1.66)
• Sleep apnea (AOR 1.52)
• Hypertension (AOR 1.36)
• Diabetes mellitus (AOR 1.18)
3. Impact of Interventions:
• Intraoperative Provocative Tests: These tests were performed in 81.9% of the cases. The leak rate was higher in patients who underwent provocative testing (0.8%) compared to those who did not (0.4%). This could be due to the trauma caused by certain testing methods.
• Surgical Drains: Drains were placed in 24.5% of the cases, and their use was associated with a higher leak rate (1.6% vs. 0.4%). This might reflect the complexity of the cases where drains are deemed necessary.
• Postoperative Swallow Studies: Performed in 41% of the cases, these studies did not show a significant difference in leak rates (0.7% for both groups).
Discussion
The study highlights that while the overall risk of gastrointestinal leaks in bariatric surgery is low, certain preoperative conditions can significantly increase this risk. The use of intraoperative provocative tests and surgical drains, often intended to detect and manage leaks early, were paradoxically associated with higher leak rates. This might be due to the selection of more complex cases for these interventions or the techniques used.
Clinical Implications
For clinicians, these findings underscore the importance of:
• Preoperative Assessment: Thoroughly evaluating and optimizing preoperative conditions such as oxygen dependency, hypoalbuminemia, sleep apnea, hypertension, and diabetes can help reduce the risk of leaks.
• Careful Selection of Interventions: While intraoperative tests and drains are valuable tools, their use should be judicious, focusing on minimizing potential trauma and selecting appropriate methods.Take Home Message
Leaks in bariatric surgery can lead to serious complications. Key points include early detection, recognizing symptoms like fever and abdominal pain, and prompt treatment to prevent severe outcomes. Preventive measures and surgical precision are crucial for patient safety.
Conclusion
Gastrointestinal leaks are a serious but relatively rare complication of bariatric surgery. By understanding the risk factors and carefully considering the use of perioperative interventions, healthcare providers can better manage and mitigate these risks, leading to safer outcomes for patients undergoing these life-changing procedures.
For more detailed insights, you can access the full study in the Journal of the American College of Surgeons here and further information on obesity surgery here.

