Table of Contents
- What is Barrett's Esophagus?
- The Study: What Did Researchers Find?
- Other Important Findings
- What Does This Mean for Patients?
- Should There Be New Guidelines?
- What Can You Do Now?
- The Bottom Line
Barrett’s Esophagus is a serious consequence of long term acid reflux. If you've undergone a sleeve gastrectomy for weight loss, you might be at a higher risk of developing a condition called Barrett's esophagus. This is the main takeaway from a recent study (the research is in press at Clinical Gastroenterology & Hepatology (doi.org/10.1016/j.cgh.2024.06.041) that has caught the attention of gastroenterology experts. But what does this mean for you, and should you be concerned? Let's break it down in simple terms.
What is Barrett's Esophagus?
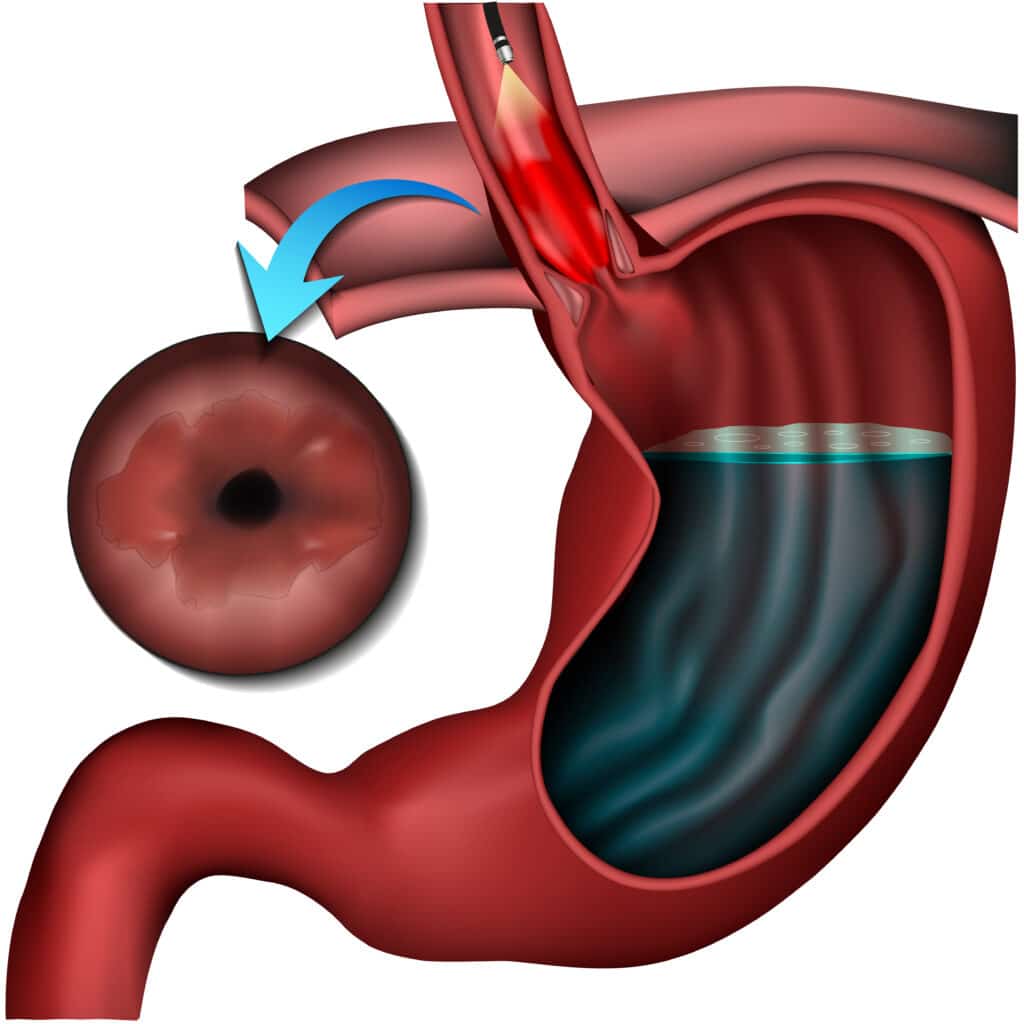
First, let's understand what Barrett's esophagus is. It's a condition where the lining of the lower esophagus (the tube that connects your mouth to your stomach) changes. This change happens because of long-term exposure to stomach acid, often due to chronic heartburn or acid reflux. While Barrett's esophagus itself isn't cancer, it can sometimes lead to a type of cancer called esophageal adenocarcinoma.
The Study: What Did Researchers Find?
Dr. Saurabh Chandan and his team looked at 17 different studies involving 1,480 patients who had undergone sleeve gastrectomy, a popular weight loss surgery. Here's what they discovered:
- Higher Risk: About 6.8% of patients developed Barrett's esophagus after sleeve gastrectomy. This might not sound like a lot, but it's significantly higher than the 0.5-2% risk in the general population.
- Time Doesn't Seem to Matter: Even when they looked at patients 10 years after surgery, the risk remained about the same (6.7%).
- Age and Weight Matter: Older patients and those with higher body mass index (BMI) before and after surgery seemed to have a higher risk.
- Gender Doesn't Affect Risk: Both men and women had similar chances of developing Barrett's esophagus after the surgery.
Other Important Findings
The study also found that after sleeve gastrectomy:
- Erosive esophagitis (inflammation of the esophagus) increased from 7.4% to 33.1%
- Hiatal hernia (when part of the stomach pushes up into the chest) increased from 13.4% to 32.1%
- GERD symptoms (like heartburn) increased from 15.3% to 50.5%
- Use of acid-reducing medications (PPIs) increased from 14% to 53.2%
What Does This Mean for Patients?
If you've had sleeve gastrectomy, these findings don't mean you'll definitely develop Barrett's esophagus. However, they do suggest that you might be at a higher risk. This information is important because it helps doctors consider whether they should recommend regular check-ups or screenings for patients who've had this surgery.
Should There Be New Guidelines?
Currently, there aren't specific guidelines in the U.S. for screening patients after sleeve gastrectomy. Dr. Chandan suggests that maybe we should consider adopting recommendations from the International Federation for the Surgery of Obesity and Metabolic Disorders. These guidelines recommend a screening endoscopy (a procedure where a camera is used to look at your esophagus and stomach) one year after surgery and then every 2-3 years after that.
However, other experts, like Dr. Tarek Sawas, believe we need more research before making official guidelines. They want to understand:
- How different risk factors work together to influence the risk of Barrett's esophagus
- How often Barrett's esophagus in these patients progresses to more serious conditions
- How weight loss from the surgery might actually help protect against cancer
- How the risk differs for various age groups and for men (since this study mostly looked at younger women)
What Can You Do Now?
While we wait for more research and potential guidelines, here are some things to keep in mind:
- Be Aware: If you've had sleeve gastrectomy, especially if you had it done outside the U.S. and aren't being followed closely by a surgeon, talk to your doctor about your risk for Barrett's esophagus.
- Consider Screening: Discuss with your doctor whether a screening endoscopy might be appropriate for you, especially if you're older or still have a high BMI.
- Manage GERD: If you're experiencing acid reflux symptoms, work with your doctor to control them. This might include lifestyle changes, medications, or in some cases, considering a different type of weight loss surgery.
- Address Other Risk Factors: Talk to your doctor about other factors that might increase your risk, like smoking, and how to address them.
- Stay Informed: As more research comes out, stay in touch with your healthcare providers about any new recommendations.
The Bottom Line
Sleeve gastrectomy is an effective weight loss surgery that has helped many people improve their health. This new research doesn't change that, but it does highlight the importance of ongoing care after surgery. It's a reminder that weight loss surgery is not a one-and-done solution, but part of a lifelong journey of health management.
If you've had sleeve gastrectomy, don't panic about these findings. Instead, use this information to have an informed conversation with your doctor. Together, you can decide on the best approach for monitoring your health and reducing your risk of complications like Barrett's esophagus.
Remember, early detection is key when it comes to conditions like Barrett's esophagus. By staying proactive about your health and working closely with your healthcare team, you can continue to enjoy the benefits of your weight loss while minimizing potential risks.
As we wait for more comprehensive studies and potential new guidelines, the most important thing is to stay engaged with your healthcare providers, report any new or worrying symptoms, and continue to make healthy lifestyle choices. Your health journey didn't end with surgery – it's an ongoing process, and you're in charge!

