Table of Contents
- Comparing VSG and ESG: Traditional Gastric Sleeve vs. Endoscopic Sleeve
- What is VSG?
- What is ESG?
- Key Differences and Similarities:
- Effectiveness and Safety
- Patient Selection and Suitability
- Costs and Insurance Coverage
- Long-term Outcomes and Research
- Conclusion
Comparing VSG and ESG: Traditional Gastric Sleeve vs. Endoscopic Sleeve
Introduction
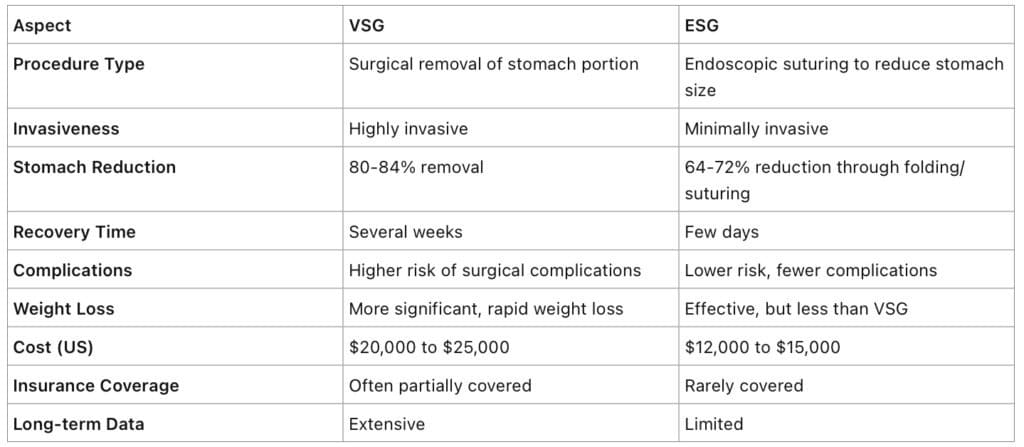
Morbid obesity remains a significant global health challenge. Among the many treatment options available, surgical interventions like Vertical Sleeve Gastrectomy (VSG) have shown considerable success in weight loss management. However, newer techniques such as Endoscopic Sleeve Gastroplasty (ESG) are emerging due to their minimally invasive nature. This blog post aims to compare VSG and ESG, highlighting their key differences, similarities, costs, and suitability for various patient needs.
What is VSG?
Vertical Sleeve Gastrectomy, commonly known as VSG, is a type of bariatric surgery that involves the surgical removal of approximately 80-84% of the stomach. This procedure leaves a smaller, tube-shaped stomach, often referred to as a “sleeve.” VSG significantly reduces the production of hunger hormones like ghrelin, leading to decreased appetite. Additionally, it enhances insulin sensitivity and leptin responsiveness, aiding in weight loss and metabolic improvements.
What is ESG?
Endoscopic Sleeve Gastroplasty (ESG) is a non-surgical, minimally invasive procedure performed using an endoscope. During ESG, a gastroenterologist places a series of sutures in the stomach to create a smaller, sleeve-like pouch without removing any part of the stomach. This reduction in stomach volume slows down the digestive process and promotes early satiety, helping patients to reduce their caloric intake effectively.
Key Differences and Similarities:
Effectiveness and Safety
VSG:
• Effectiveness: VSG patients typically experience significant weight loss, often losing 60-70% of excess weight within the first year. The procedure also improves or resolves obesity-related comorbidities such as type 2 diabetes, hypertension, and sleep apnea.
• Safety: As a major surgery, VSG carries risks such as infection, bleeding, and nutrient deficiencies. Long-term monitoring and lifestyle changes are crucial for maintaining health post-surgery.ESG:
• Effectiveness: ESG results in substantial weight loss, with patients losing around 18-20% of their total body weight within a year. This is less than VSG but still significant for improving health outcomes.
• Safety: ESG has a lower risk profile compared to VSG, with common side effects including mild nausea and abdominal discomfort. Severe complications are rare.
Patient Selection and Suitability
Choosing between VSG and ESG depends on various factors, including a patient’s health status, weight loss goals, and personal preferences.
VSG:
• Ideal Candidates: Patients with a BMI over 40 or those with a BMI over 35 with obesity-related health issues. It’s also suitable for patients who prefer a one-time, permanent solution.
• Considerations: Patients must be prepared for a significant lifestyle change and long-term follow-up care.ESG:
• Ideal Candidates: Patients with a BMI of 30-40 who have not succeeded with diet and exercise alone. It’s also a good option for those seeking a less invasive procedure.
• Considerations: Patients need to be committed to a structured weight loss program post-procedure to maintain results.Costs and Insurance Coverage
The financial aspect is a critical consideration for many patients.
VSG:
• Cost: In the US, VSG typically costs between $20,000 and $25,000. Some insurance plans may cover part of the expense, especially if the surgery is deemed medically necessary.
• International Options: In countries like Mexico, the cost can be significantly lower, often ranging from $5,000 to $10,000.ESG:
• Cost: ESG costs range from $12,000 to $15,000 in the US. However, it is rarely covered by insurance, making it a more out-of-pocket expense for patients.
• International Options: Similar to VSG, undergoing ESG in countries like Mexico can reduce the cost substantially.Long-term Outcomes and Research
Long-term studies and research are vital for understanding the sustainability of weight loss and overall health benefits.
VSG:
• Long-term Success: Patients generally maintain significant weight loss for years post-surgery. Studies show that VSG can lead to sustained improvements in metabolic health and quality of life.
• Research: Extensive data supports VSG’s efficacy and safety, making it a well-established option for severe obesity.ESG:
• Long-term Success: While ESG shows promising short- to mid-term results, long-term data is still emerging. Most patients maintain significant weight loss for at least two to three years.
• Research: Ongoing studies are needed to further validate ESG’s long-term effectiveness and safety profile.Conclusion
Both VSG and ESG offer effective solutions for weight loss, each with unique benefits and considerations. VSG is a more established procedure with extensive data supporting its use, especially for patients with higher BMI and obesity-related comorbidities. ESG provides a less invasive alternative with a quicker recovery and lower risk of complications, making it an attractive option for many.
Understanding the differences, costs, and long-term outcomes of these procedures can help patients make informed decisions about their weight loss journey. Consulting with a healthcare provider is crucial to determine the best approach based on individual health needs and goals.
For more details, contact us.

